What Is Fatty Liver Disease?
Fatty Liver Disease (also called hepatic steatosis) occurs when too much fat builds up in the liver. While it’s normal for the liver to contain some fat, excess fat can lead to inflammation, scarring, and long-term liver damage if left untreated.
There are two main types:
- Nonalcoholic Fatty Liver Disease (NAFLD): Fat buildup not caused by alcohol use.
- Alcohol-Associated Fatty Liver Disease (AFLD): Caused by heavy or long-term alcohol use.
Over time, fatty liver can progress to nonalcoholic steatohepatitis (NASH), fibrosis, cirrhosis, or even liver failure if it’s not identified and managed early.
Common Symptoms of Fatty Liver Disease
Fatty liver disease is often called a “silent condition” because most people have no noticeable symptoms in the early stages. However, as the condition progresses, you might notice:
- Fatigue or low energy
- Discomfort or dull pain in the upper right abdomen
- Unexplained weight loss
- Weakness or general feeling of being unwell
- Mild nausea or poor appetite
Hidden or Subtle Signs to Watch For
Because early fatty liver often goes unnoticed, it’s important to recognize less obvious symptoms that can indicate your liver is under stress:
- Brain fog or difficulty concentrating – the liver’s reduced ability to filter toxins can affect mental clarity.
- Unexplained skin changes – such as dark patches (especially on the neck or underarms), redness on the palms, or small clusters of blood vessels (spider veins).
- Abdominal bloating or feeling “full” quickly after eating – due to fluid buildup or an enlarged liver.
- Unexplained weight gain, especially around the midsection.
- Swelling in legs or ankles (edema).
- Changes in mood or sleep – liver dysfunction can affect hormone balance and metabolism.
These signs can be subtle and easy to overlook, which is why routine checkups and blood tests are so important.
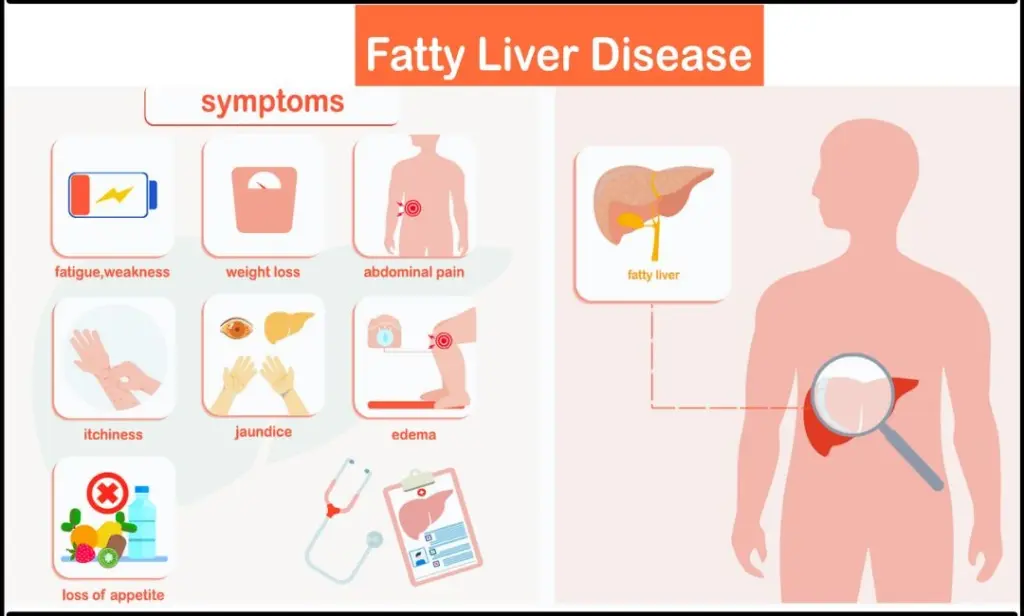
Image Source: Continental Hospitals
How Fatty Liver Is Diagnosed
Fatty liver disease is often found incidentally during routine bloodwork or imaging. Your provider may use:
- Liver function tests (ALT, AST)
- Ultrasound or FibroScan to measure fat and stiffness in the liver
- CT or MRI imaging
- Liver biopsy (in select cases) to confirm inflammation or fibrosis
Why Early Detection Matters
When detected early, fatty liver can often be reversed with lifestyle changes and proper medical care. Early management can:
- Prevent progression to liver scarring or cirrhosis
- Improve energy, metabolism, and overall health
- Reduce risks for diabetes, heart disease, and other metabolic conditions
How to Support Liver Health
Simple steps can make a big difference:
- Maintain a healthy weight
- Eat a balanced diet rich in vegetables, whole grains, and lean proteins
- Limit sugar, refined carbs, and processed foods
- Engage in regular physical activity
- Avoid excessive alcohol and unnecessary medications
- Schedule regular checkups with your healthcare provider
When to Talk to Your Provider
If you experience ongoing fatigue, abdominal discomfort, unexplained weight changes, or any of the hidden symptoms listed above, it’s important to discuss them with your healthcare provider.
At Verity Health PNW, we’re committed to helping you identify and manage liver concerns early — supporting your journey toward long-term health and wellness.
Comparison Table
Symptoms of Fatty Liver Disease Comparison Table
Medical professionals rely on systematic assessment to identify fatty liver disease patterns. We have organized the twelve warning signs to help you understand their characteristics and clinical significance.
| Symptom | Key Characteristics | Primary Mechanism | When to Seek Help | Prevalence (if mentioned) |
|---|---|---|---|---|
| Fatigue and Weakness | Debilitating weariness that persists despite rest; affects physical and mental clarity | Liver inflammation disrupting CNS communication; altered melatonin production | When exhaustion persists despite rest or interferes with daily activities | 50-85% of chronic liver disease patients |
| Mild Abdominal Discomfort | Dull or aching pain in upper right abdomen; feeling of fullness | Liver enlargement causing pressure on liver capsule | Persistent pain that doesn’t resolve with rest; severe sudden pain | Not mentioned |
| Unexplained Weight Changes | Sudden weight gain or loss without lifestyle changes | Decreased liver function affecting metabolism; insulin resistance | Weight changes of 5% or more within months | Over 50% experience significant changes within 1-2 years |
| Elevated Liver Enzymes | Increased ALT, AST, ALP, and GGT levels in blood | Liver cell damage causing enzyme leakage into bloodstream | Any elevation in liver enzymes, even without symptoms | Most common cause of elevated enzymes in US adults |
| Dark Urine | Brown or tea-colored; clear despite dark color | Disrupted bile flow leading to bilirubin buildup | Persistent dark urine despite hydration | Not mentioned |
| Red Palms | Symmetrical redness in palms; warm to touch; blanchable | Elevated estrogen levels causing blood vessel dilation | Persistent redness with other liver symptoms | 23% of cirrhosis patients |
| Swelling in Legs/Ankles | Soft, painless swelling; leaves temporary indentation | Portal hypertension causing fluid leakage | Swelling that doesn’t improve with elevation | 50% within 10 years of cirrhosis |
| Cognitive Issues | Memory problems; poor concentration; personality changes | Toxin buildup in brain; chronic inflammation | Increasing confusion or disorientation | Up to 70% of NAFLD patients |
| Persistent Upper Right Pain | Sharp, stabbing sensations under right ribcage | Liver enlargement pressing on Glisson’s capsule | Severe pain interfering with daily activities | One-third of NAFLD/NASH patients |
| Itchy Skin | Generalized itching worse at night; no visible rash initially | Bile acid accumulation in bloodstream | When itching interferes with sleep or daily activities | 20% of NAFLD patients |
| Jaundice | Yellowing of skin and eyes; dark urine; light stools | Bilirubin buildup due to impaired liver function | Immediate medical attention needed | Not mentioned |
| Spider Veins | Web-like red/blue patterns with central red spot | Hormone imbalance causing blood vessel dilation | When multiple spider veins appear (>3) | 95% specificity for chronic liver disease |

Verity Health looks forward to supporting your liver wellness journey. Our comprehensive services include metabolic health guidance and personalized treatment approaches.
We believe in empowering community health through early detection and evidence-based care.
Your liver health matters to your overall wellbeing. Schedule a consultation if you’ve noticed any of these symptoms or have risk factors like diabetes or family history.
We look forward to helping you protect your liver function and enhance your health for years ahead.
FAQs
Q1. What are the early warning signs of fatty liver disease? Early signs include persistent fatigue, mild abdominal discomfort in the upper right quadrant, and unexplained weight changes. However, many people with fatty liver disease don’t experience noticeable symptoms in the early stages, which is why regular check-ups are important.
Q2. How does fatty liver disease affect cognitive function? Fatty liver disease can impact cognitive function by causing memory problems, difficulty concentrating, and even personality changes. This occurs due to toxin buildup in the brain and chronic inflammation associated with liver dysfunction.
Q3. Can fatty liver disease cause skin changes? Yes, skin changes can be indicators of fatty liver disease. These may include jaundice (yellowing of skin and eyes), itchy skin without a visible rash, red palms, and the appearance of spider veins, particularly on the face, neck, and upper chest.
Q4. Is weight gain always associated with fatty liver disease? While weight gain is common, fatty liver disease can also cause unexplained weight loss in some cases. Significant weight changes in either direction without changes to diet or exercise routines can be a sign of liver dysfunction.
Q5. How is fatty liver disease diagnosed? Fatty liver disease is often initially suspected due to elevated liver enzymes in routine blood tests. Further diagnosis may involve imaging tests like ultrasound or FibroScan, which can assess liver fat content and stiffness non-invasively. In some cases, a liver biopsy may be necessary for definitive diagnosis.